Australian injury trends from venomous bites and stings over 13 years. Ronelle Welton featured academic in Pursuit article
Anaphylaxis found to be responsible for the most morbidity and mortality following envenomation events

This article was first published on Pursuit. Read the original article.”
Venomous stings and bites lie close to home
The first national study of the bites and stings inflicted by Australia’s venomous creatures shows our towns and cities are a hotspot for deadly encounters.
The 13 years of data also reveals that of all Australia’s creepy crawlies, it is bees and other insects – not snakes, spiders, or jellyfish – that pose the biggest public health threat. But snakes are the country’s deadliest venomous creature.
This stereotype-shattering research, published in the Royal Australian College of Physicians’ Internal Medicine Journal, changes what we thought we knew about Australia’s venomous creatures.
“Australia has an international reputation for being the epicentre of all things venomous, whether it’s snakes and spiders on land, or lethal jellyfish, stingrays, stonefish and octopi in our oceans,” says lead researcher Dr Ronelle Welton, a public health expert with the Australian Venom Research Unit at the University of Melbourne’s Department of Pharmacology.
“Yet until now, there has been a real lack of data about where venomous injuries occur, the reasons why they happen and what happens after a person is bitten.”

Including fatalities, venomous stings and bites resulted in almost 42,000 hospitalisations over the study period. Bees and wasps were responsible for just over one-third (33%) of hospital admissions, followed by spider bites (30%) and snake bites (15%).
In all, 64 people were killed by a venomous sting or bite, with over half of these (34) caused by an allergic reaction to an insect bite causing anaphylactic shock. Of these, 27 deaths were the result of a bee or wasp sting, with only one case of a beekeeper being killed.
But snake bites also caused 27 deaths. Snake bite envenoming caused nearly twice as many deaths per hospital admission than any other venomous creature.
Tick bites caused three deaths and ant bites another two. There were no spider bite fatalities. A man died from a red back spider bite in April 2016, the first spider bite death in more than 30 years, however this was outside the study period.
| Creature | Deaths (2000-2013) | Hospitalisations (2001-2013) |
|---|---|---|
| Snakes | 27 | 6,123 |
| Hornets, wasps and bees | 25 bees, 2 wasps | 12,351 |
| Spiders | 0 | 11,994 |
| Ticks and ants | 5 | 4,533 |
| Marine animals | 3 | 3,707 |
| Scorpions | 0 | 61 |
| Centipedes / millipedes | 0 | 119 |
| Unknown animal or plant | 2 | 536 |
Surprisingly, over half of these deaths happened at home, and almost two-thirds (64%) occurred not in the isolated areas we might expect, but rather in major cities and inner-regional areas where healthcare is readily accessible.
Western Australia and South Australia recorded the highest number of recorded fatal stings and bites over the decade, while Tasmania was the only state or territory where no deaths were recorded. Bites and stings were most likely to occur between April to October.
The study is the first large-scale audit of death and injury from envenoming ever undertaken in Australia.
Dr Welton and her colleagues examined hospital data from the Australian Institute of Health and Welfare (AIHW) and mortality data from National Coronial Information System from August 2001 to May 2013, as well as Cause of Death Unit Record Files collated by the AIHW.
Danger of anaphylaxis
Researchers believe one of the reasons that anaphylaxis from insect stings has proven deadly may be because people are complacent in seeking medical attention and anaphylaxis can kill quickly.
While three-quarters of snakebite fatalities at least made it to hospital, only 44 per cent of people who died from an allergic reaction to an insect sting got to hospital.
“Bees are a ubiquitous creature that we are accustomed to seeing. Perhaps it’s because bees are so innocuous that most people don’t really fear them in the same way they fear snakes,” Dr Welton says.
“Without having a previous history of allergy, you might get bitten and although nothing happens the first time, you’ve still developed an allergic sensitivity. We need to understand why people are dying from bee sting anaphylaxis at home.”
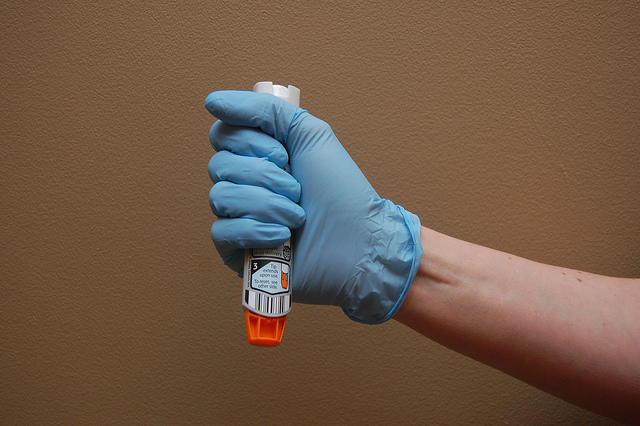
Professor Daniel Hoyer, who heads up the University of Melbourne’s Department of Pharmacology and Therapeutics, says it could be lack of access to adrenaline auto-injectors used to treat anaphylactic shock, also known as Epipens.
“The number one surprise in this research is there are so many bites from insects,” Professor Hoyer said. “The majority of serious envenoming incidents involved anaphylactic shock. I suspect the incidence of allergy is enormous in this country.
“We observed this during the recent asthma storm, when over 8500 patients showed up in the emergency room in hospitals around Melbourne and at least eight died, yet many of these people did not know about their susceptibility to strong allergic reactions or asthma status. We need to ask why don’t people at risk have Epipens at home?”
Given there are 140 species of land snakes in Australia, snake bite fatalities are very rare, at 27 for the study period. To put that in perspective, 100,000 people die from snake bite globally each year.
While it’s natural to be frightened of snakes, Dr Welton says the reality is, a person is more likely to die from an encounter with a horse or a dog.

Since 2000, 74 people have died from being thrown or trampled by a horse. Twenty-six people have died from shark attack and 23 from altercations with dogs. Crocodiles have been responsible for 19 deaths.
And compared to 4,820 drowning deaths and 974 deaths from burns in the same period, the snake bite figures figures are still remarkably low.
Young men are most at risk
Men aged 30 to 35-years-old are most likely to be bitten or stung, followed closely by the five to nine-year-old age group, which Professor Hoyer says may reflect greater risk taking behaviour among men and boys.
“There is a massive discrepancy between men and women that starts very early,” Professor Hoyer adds. “Even between the ages of zero and four-years, boys are suffering bites and stings more frequently than girls and this is across the age spectrum until 75 when it evens out.
“When you consider the highest age groups were between 25 and 45, we can assume risk taking-behaviour is more common in men – it could be that blokey culture is driving it.”
Snakes are city-slickers too

Waiting for the Tiger mosquito
Dr Welton said she was surprised to see a pattern of snake bites across the populous coastal areas of Australia.
“A snake bite is usually thought of as an outdoor medical emergency, but our data showed the majority of snake bite fatalities occur around a person’s residence within the major city or inner regional area,” Dr Welton says.
“The big question is how can we manage this co-existence without being detrimental to people and the creatures themselves? For me, it comes down to understanding, education, prevention and first-aid.
“Giving people advice to wear boots in the bush and make lots of noise to avoid snake bite isn’t good enough. It’s everyone’s responsibility to learn first aid, particularly pressure-immobilisation, which can be applied for a range of injuries when it comes to animals.

“And don’t try to kill the snake. In numerous cases, that’s when people get bitten. Go to your council website, find a snake catcher, put the number on your fridge. Make sure you’re prepared.”
In numerous cases, that’s when people get bitten. Go to your council website, find a snake catcher, put the number on your fridge. Make sure you’re prepared.”Marine stingers NOT as big a threat as we imagine
The study was limited to those deaths actually recorded as being caused by envenoming and Dr Welton noted “the information reviewed was only as accurate as the information entered, and some records may not have made it into the national dataset.
According to the data there were only three recorded marine stinger fatalities in the study, all of them box jellyfish.
Dr Welton believes the public safety messaging around jellyfish management has been very effective.
“From a jellyfish perspective, there has been a huge public health intervention and yet for bees and snakes, not so much,” she says. “You have the tourism industry, the fisheries industry, surf lifesaving, all with a stake in jellyfish sting prevention who champion this need. Linking up these industries and health networks would help track cases, for example Irukandji stings have been recorded progressing down the Queensland coast for some years.”
“When you look at how comprehensive awareness campaigns are about jellyfish stings in certain parts of Australia, compared to bee sting anaphylaxis which can happen everywhere, the public health approach is certainly not as focussed.”
Australian guidelines must be reviseD
Dr Welton believes the current national guidelines for prevention and treatment of envenoming is inadequate because we actually know very little about the health burden of venomous creatures.

The new battlefront in malaria research
“From a public health perspective, we can’t make informed decisions until we have a much clearer picture about what’s going on,” she says.
“For example, in South Australia, there are a lot more stings and anaphylaxis from bees. In Queensland there are more snake bites. In Tasmania, their biggest issue is jumper ant anaphylaxis. So the clinical management needs to vary for each state and territory.”
She says the new state-based Primary Health Care networks, which coordinate hospitals, GPs and other health services, would be a good start. Current first aid practices are another area that could be re-examined, she says.
“We are aware that people aren’t using pressure immobilisation effectively. We want to know if that’s because it is too complicated and whether it is even necessary. Perhaps the key message should be that if people can get to a hospital, just get to a hospital.”
Banner Image: Fractality/Flickr