Liver-secreted protein may hold key to new link between liver disease and type 2 diabetes
Montgomery and Watt Labs identify a new protein called Arylsulfatase A (ARSA), which improves insulin sensitivity and blood glucose control.
Department of Anatomy and Physiology researchers have inched closer to determining whether ARSA can be used as a new treatment for type 2 diabetes.
Following the world’s most comprehensive assessment of changes in protein secretion from the liver in the presence of advanced liver disease, the findings were published in Nature Communications this week.
The research, led by Dr Magda Montgomery and Professor Matt Watt, described global changes in protein secretion in non-alcoholic steatohepatitis (NASH) and identifies ARSA as a regulator of liver to muscle communication – and as a potential therapeutic target for type 2 diabetes.
L-R: Prof Matt Watt, Dr Ben Parker, Dr Magda Montgomery, Dr Paula Miotto, Mr Will de Nardo, Dr Stacey Keenan and Dr Jackie Bayliss.
“We are working to understand how the presence of advanced liver disease, or NASH, contributes to the development of insulin resistance and type 2 diabetes – and how to target those changes to improve health outcomes,” said Dr Montgomery.
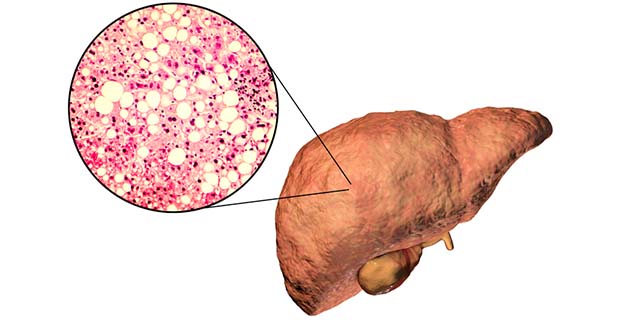
“Fat accumulation in the liver, known as non-alcoholic fatty liver disease (NAFLD), affects around 25 per cent of the global population, which means every fourth person has some form of NAFLD.
“If you are obese or have type 2 diabetes, your chance of having NAFLD increases to 50 to 80 per cent.”
The problem is, fatty liver can progress to more advanced liver disease, including NASH, liver fibrosis, cirrhosis and liver cancer.

The liver, as an important endocrine organ, secretes thousands of proteins, lipids and nucleic acids, and this secretion is highly impacted by NAFLD and NASH.
“Proteins secreted from the liver impact many other tissues, including your muscles, heart and brain in both positive and negative ways, and investigating protein secretion in various disease states will increase our understanding of metabolic regulation on a whole-body level,” explained Dr Montgomery.
In a previous study, the Montgomery and Watt research teams showed that another liver-secreted protein, SMOC1, which is also increased in NAFLD, improves blood glucose control and is a potential novel therapy for type 2 diabetes.
This week’s paper extends on the SMOC1 findings by providing detailed information on liver-secreted proteins in advanced liver disease, and on identifying a further protein that regulates blood glucose control.
To find out more, we asked the Dr Montgomery, a NHMRC CDF1 Fellow, to answer our top five questions about her research and what will happen next.
1. What is NASH?
Non-alcoholic fatty liver disease (NAFLD), in simple terms, is the accumulation of fat in the liver. It is the world’s most common chronic liver condition, affecting around 25 per cent of the global population. Simple steatosis can further progress to advanced liver disease, including non-alcoholic steatohepatitis (NASH), cirrhosis and hepatocellular carcinoma. This can lead to liver failure and liver transplantation. It increases in parallel with obesity and type 2 diabetes – prevalence is estimated at 57 to 64 per cent in obesity and 37 per cent in type 2 diabetes. The factors linking NASH with these metabolic diseases are still unknown.
2. What is ARSA?
Arylsulfatase A (ARSA) is hepatokine or protein which is released from the liver into the blood.
ARSA improves insulin sensitivity. Our findings show having more ARSA in the liver improves blood glucose control by increasing glucose uptake into muscle. This happens by ARSA inhibiting the release of lysophospholipids from the liver into the blood, with these changes improving muscle glucose uptake. It is a novel finding into the mode of communication between these tissues.
3. Why are your recent findings important?
We identified around 2800 proteins released from livers of mice with NASH, and found that factors such as proteins, lipids and nucleic acids secreted from NASH livers induce insulin resistance and various defects in glucose and lipid metabolism in muscle, liver or adipose tissue. This highlighted that the NASH livers impacts metabolic health on a whole-body level.
Our study specifically identified a novel liver-secreted protein called ARSA, which is increased in both mice and humans with NASH. Secretion of ARSA is also increased in patients with type 2 diabetes, which means that it might play a role in blood glucose control.
The research shows that ARSA is important for inhibiting the release of specific lipids from the liver called lysophospholipids, and thereby for reducing blood levels of these lipids. These lipids can be detrimental and induce insulin resistance on a systemic level. Put simply, having more ARSA in the liver is a good thing as ARSA inhibits the release of these lysophospholipids, and improves insulin sensitivity – particularly in muscle.

4. How will this research help those with insulin resistance and type 2 diabetes?
Our research shows that increasing ARSA – either in the liver through gene therapy, or in the blood through protein therapy (injections of ARSA protein) – may potentially be a viable strategy for the treatment of insulin resistance and type 2 diabetes. We show that both strategies work well in type 2 diabetic mice in improving blood glucose control.
5. What are the next steps?
To advance towards therapeutic development, more pre-clinical studies are needed, including further validation of the longer-term impact of increased ARSA in the liver and blood.
ARSA protein and gene therapy has previously been shown to be a safe therapeutic approach for metachromatic leukodystrophy in humans, and future studies are warranted to assess the potential for ARSA as a therapeutic strategy for the treatment of type 2 diabetes.

Researchers involved
Prof Matt Watt, Dr Ben Parker, Dr Magda Montgomery (above), Dr Paula Miotto, Mr Will de Nardo, Dr Stacey Keenan, and Dr Jackie Bayliss.
Biomedical Precinct links
- Mass Spectrometry and Proteomics, Bio21 Molecular Science and Biotechnology Institute (Bio21 Institute)
- Australian Centre for Accelerating Diabetes Innovations Research Centre (ACADI)
Funded by
- National Health and Medical Research Foundation of Australia
- The Diabetes Australia Research Trust
- Research Fellowships from the NHMRC